Becoming a Hospital of the Future: 4 Focus Areas for Your Organization to Become Operationally Efficient and Optimize Growth
As healthcare becomes increasingly boundaryless, the demand for integration, and the availability of care outside of the four walls of the traditional hospital is critical. In parallel with this market dynamic, hospitals are under increasing pressure to remain operationally sustainable.
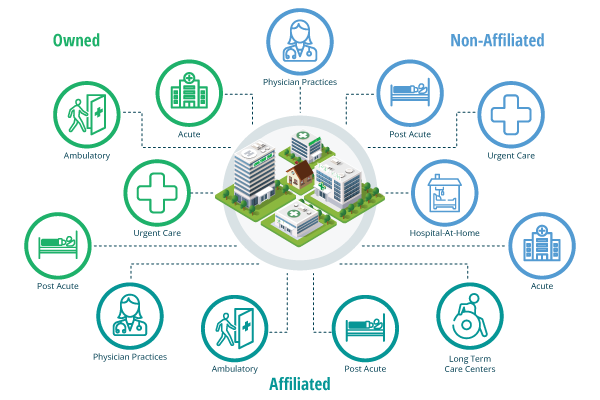
With this distribution of care across multiple settings, network-wide orchestration will take on increased importance, evolving to an integrated ecosystem that centralizes functions to create an efficient and uniform experience for patients.
There is a battle going on in healthcare to manage the patient through the ecosystem. The payer would like it to be them, but few patients trust insurance companies. Within the physician community, PCPs and others want to be the quarterback of care. I believe health systems have the best visibility and scope, not to mention consumer trust, to remain the epicenter of care, acting as the integrated and central hub for wider care delivery.
Below I’ll outline four areas I think can help hospital leaders define a path towards becoming an operationally sustainable organization designed to optimize growth and expand the capacity to care.
Operational efficiency
Other industries rely on workflow automation and data-driven optimization to remove inefficiencies and optimize growth opportunities – shouldn’t healthcare? Today, patient care is riddled with disconnected and inefficient processes that impact patient experience and outcomes. With the shift towards a more boundaryless care model, connecting operations within and across a hospital, health system, and health network will become even more important to orchestrate care efficiently and effectively. Hospitals must adopt an Operational Platform that compliments their Electronic Medical Record, providing clear differentiating value, including:
- Automated and optimized workflows across care settings
- Improved resource utilization
- Streamlined and shared patient access, care delivery, and transition journeys
- Data-backed proactive planning dashboards powered by both historic and predictive data
Data driven clinical excellence
The importance of measuring what matters has never been more prevalent. With competition at an all-time high, pairing clinical and operational excellence is top of mind for every hospital executive. The focus should be around integrating a hospital’s Operational Platform with their EMR to allow for shared visibility and collaboration across a wider network of care delivery. The Operational Platform informs the network where the patient is going and what resources are needed while the EMR manages their clinical documentation and billing in parallel. Underpinned by data collection and with a shared feedback loop, hospitals can start to measure the end-to-end patient care journey.
Patient-centric model
Every patient is an opportunity for a hospital to grow its network. Hospital leaders must think strategically about care access, care delivery, and care transitions so they form an integrated model for the patient throughout their journey. This includes reimagining patient flow by integrating tools like remote patient monitoring, alongside your organizations Operational Platform and EMR to allow patients to take a more proactive role in managing and understanding their care journey.
Co-opetition
A term new in healthcare, co-opetition is the move towards collaboration amongst historically competitive organizations. With patients taking more control of their care delivery, hospitals and health systems must work more collaboratively with their neighbors to ensure that the patient gets the right care, in the right places, with the right resources.
Becoming operationally sustainable and optimizing growth opportunities will require an integrated and boundaryless approach by hospital leaders. The patient journey is not linear; they move (not so seamlessly) between ambulatory, in-patient and post-acute. Having visibility to patients, capacity, staffing and so much more across all settings is no longer a nice to have but mission critical for health systems. Those that take on this challenge will not only be operationally sustainable, but they will thrive.

About the expert
Nigel Ohrenstein
President
Serving as President, Nigel Ohrenstein has extensive experience as a founder and healthcare entrepreneur with more than 20 years of proven success building and developing a vision for the business that will improve outcomes and build a stronger, more sustainable healthcare system for patients and clinicians alike.
Prior to joining TeleTracking, Nigel served as President of Kaia Health, a clinically validated MSK solution, where he helped significantly increase revenue as well as product activation and retention. Before Kaia Health, Nigel was a Co-Founder at Lumeris, a leading provider of technology, insurance capabilities and expertise to support health systems and payers as they transitioned to value-based care.
Nigel holds both a BA and MA in Law from Cambridge University and attended College of Law, London.
